 Am I the only one who wished there was a “How-to-Do-Life-During-a-Global-Pandemic-for-Dummies” handbook at the initial outbreak of COVID-19? There were so many unknowns: “How am I going to buy groceries?”, “What do I do about my son’s doctor appointments?”, “Do I have to wear a mask?”, and most importantly – “Will they EVER go back to school?!” I jest (only slightly). I’m a natural-born rule-follower, people-pleaser, and social butterfly; so as you can imagine, it was quite the daily emotional conundrum for me.
Am I the only one who wished there was a “How-to-Do-Life-During-a-Global-Pandemic-for-Dummies” handbook at the initial outbreak of COVID-19? There were so many unknowns: “How am I going to buy groceries?”, “What do I do about my son’s doctor appointments?”, “Do I have to wear a mask?”, and most importantly – “Will they EVER go back to school?!” I jest (only slightly). I’m a natural-born rule-follower, people-pleaser, and social butterfly; so as you can imagine, it was quite the daily emotional conundrum for me.
However, now that we’ve had some time under our belts with living life during the COVID-19 pandemic, we’ve all made daily changes to adjust to the “new normal.” There are changes I’ve made that I never anticipated as a result of the pandemic, like sending my kids to school wearing masks, waiting in my car during my son’s therapy sessions, and attending church in an individual’s home. My expertise in life is being a mom and taking care of our house, so I had to quickly learn how to do that safely given the new circumstances of the pandemic. It’s my job to help my children safely navigate life in the midst of the pandemic.
Chances are high your healthcare facility doesn’t look anything like what it did prior to the pandemic, and although it’s your comfort zone and area of expertise, your patients may still have some unknowns that are inhibiting them from returning to your office. As patients are starting to adjust to the “new normal,” they need your help to safely navigate the area of healthcare in their lives.
 Uncharted Waters
Uncharted Waters
Patients obviously took a hiatus from visiting healthcare facilities during the initial outbreak of COVID-19, but according to a recent report from the Center for Disease Control, an estimated forty-one percent of Americans say they’ve recently delayed or avoided seeking routine or emergency care due to COVID-19 related concerns. (1) As discussed in last week’s blog, with all the COVID-19 related changes, your patients are likelier than ever to have some anxiety regarding visiting their doctor’s office. They might be wondering, “Am I going to come into contact with the virus?”, “What will the waiting room look like?”, “Does my medical need require immediate attention, or can it wait?”, “Will I increase the risk of exposure of the virus to others?” While the mid-COVID-19-doctor’s-office may be your new daily norm, it’s still unchartered waters for many of your patients and potentially a source of fear or anxiety.
 Worsening Conditions
Worsening Conditions
This presents a new problem for both patients and physicians. Patients’ health issues are worsening or going completely undetected due to patients not receiving timely care out of COVID-19 related concerns. In his news article for AMA, author Marc Zarefsky notes, “About one in ten adults admitted that their condition or the condition of their family member worsened by not getting care when it was originally scheduled.” (2)
During her interview with author Shelley Kofler, lead radiologist for breast imaging at University Health, Dr. Pam Otto, says, “Mammogram screenings in April 2020 plummeted 89% across the country compared to April 2019. The number of newly diagnosed breast cancers that typically result from those screenings dropped 48%. That means there are women with malignant tumors who are not getting early treatment, and their cancers are growing undetected.” (3)
To make matters worse, according to a survey done by the CDC in late June, individuals with disabilities and those with two or more underlying health conditions were among the majority of people who put off medical care. (4)
 Bad Assumptions
Bad Assumptions
During the pandemic I canceled all non-emergent healthcare appointments for my children, including their well-checkups with their pediatrician. Obviously my main motive was to avoid exposing them to the virus, but I also thought I was doing our pediatrician a favor by lightening her load, assuming she was probably overwhelmed with COVID-19 related cases. I finally gave them a call when the stubborn wart on my son’s finger became offensively large. Upon calling, I had so many questions: “What does your waiting room experience look like?”, “Do we need to wear masks?”, “Will I be filling out any paperwork?”, “Does Dr. X even see non-emergent patients right now?” The staff was very thorough in answering all my questions and I was able to set appropriate expectations for our upcoming visit. Furthermore, the pediatrician kindly brought clarity to my false assumption by informing me that they had not been swamped with COVID-19-related cases; on the contrary – most families had been steering clear of her office. Consequently, her schedule for well checkups was completely backlogged due the amount of families who put off their originally scheduled appointments. I was shocked at how incorrect my assumptions were. My personal experience causes me to wonder how many of your patients haven’t returned to your office simply because they’ve made incorrect assumptions, too.
My suspicions are confirmed in Marc Zarefsky’s previously mentioned AMA article. While interviewing two physicians on the specific topic of pediatric care during the pandemic, he writes, “Drs. Harris and Goza said parents should make sure to schedule routine well-child visits with their child’s pediatrician.” (2)
 Proactive and Thorough Communication
Proactive and Thorough Communication
Your healthcare facility probably looks very different than what it used to and the fear of the unknown can be inhibiting your patients from returning. Personally speaking, our mid-pandemic pediatrician’s office felt like a completely different experience than pre-pandemic. Patients want to know first, what changes have been made to ensure their safety, and secondly, what they can expect in regards to those changes when they return to your office. It’s crucial that healthcare facilities be proactive and thorough in communicating with their patients.
Stephanie Cajigal’s article, “How to Make Your Patients Feel Safe Enough to Come Back During the COVID-19 Pandemic” caught my attention. In it, she records Dr. Gavin Setzen’s testimony at Albany ENT and Allergy Services in Albany, NY. She explains how they returned to their pre-pandemic patient volume as soon as July of this year. She writes, “Dr. Setzen credited part of the increase in volume to a communication strategy the practice developed to inform patients, referring physicians, and staff that they are open and adhering to new safety standards. He said the practice’s marketing team has been sending patients’ text and email updates about these changes and posting about them on the practice’s website and social media accounts. Staff members have also reached out to patients to reschedule appointments that were cancelled during shelter-in-place orders.” (5)
 A Great Example
A Great Example
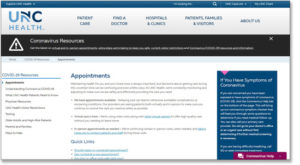
Check out UNC Health for a great example of communicating clearly to help their patients navigate visiting their facility mid-pandemic. They clearly list that they are indeed booking appointments. They specifically list options for care treatment such as virtual or in person. They practically answer a lot of the questions I listed above regarding returning to the pediatrician’s office. UNC Health seems to have a real beat on what patients are wondering right now, and they are being proactive in educating them. (6)
Chances are you’ve already made changes within your clinic to ensure the safety of your patients and staff by now. Do your patients know about those changes? Personally speaking, I know if my pediatrician’s office had reached out to me first to inform me they were still safely performing well checkups, I would have scheduled my children’s appointments long before I actually did. Patients need your help in knowing how to navigate their healthcare during this “new norm.” It could be as simple as creating and sending out a mass email with helpful information regarding the changes you’ve made in your facility. How can you increase communication to your patients to inform them of those changes and to help them set appropriate expectations regarding how to navigate those changes? Please comment below with any tips or advice if you’ve experienced success with communicating mid-pandemic changes and assurances to your patients!
Please let us know if you have comments or questions, and subscribe to our Email Updates, so that you can be assured to receive Thinking Thursdays TIPs.
Thank you!
Jerry
Jerry L. Stone
Co-Founder/COO
MedicalGPS, LLC.
Resources:
- https://www.mclaren.org/main/news/millions-of-americans-are-delaying-health-care-dur-2971
- https://www.ama-assn.org/practice-management/sustainability/half-adults-know-care-was-postponed-during-covid-19
- https://healthfocussa.net/cancer/mammograms-catch-breast-cancer-early-and-save-lives/
- https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a4.htm
- https://www.enttoday.org/article/how-to-make-your-patients-feel-safe-enough-to-come-back-during-the-covid-19-pandemic/
- https://www.unchealthcare.org/coronavirus/appointments/

